|
Fifth Dimension Catalog Contact Us |
|

|
Side Effects of Brain Irradiation |
Brain metastasis is unfortunately a common complication of metastatic breast and lung cancer. The diagnosis is usually made after a patient may develop neurologic symptoms such as a headache or nausea. The diagnosis is often confirmed by radiographic tests such as CT scan or MRI of the brain. Evaluation of cerebrospinal fluid (fluid around the brain) can also be used to help diagnose brain tumors, if tumor cells can be identified under the microscope. There is also new evidence that specific proteins within the cerebrospinal fluid can also be used to help diagnose brain metastatic breast and lung cancer as well as non-Hodgkin's lymphoma. (Roy et al., 2007 J Clinical Oncology, in press).
Radiation treatment of metastases to the brain can be highly effective therapy which results in tumor shrinkage and symptom improvement more than 50% of the time. The most common type of treatment is known as whole brain radiation; this approach treats the entire brain so that multiple metastasis involving both small and large tumor lesions are affected, as well as areas of normal brain. Surgical treatment of brain metastasis also has an important role, especially if there is only one tumor in the brain or if a tumor site is compressing a particularly important area of the normal brain and causing significant symptoms. Surgical treatment is commonly administered with radiotherapy. Thus, brain radiotherapy is the most significant treatment given its ability to cause tumor shrinkage in a short period of time, typically within days to weeks.
However, radiotherapy to the brain is often associated with significant side effects. These side effects may occur in three distinct phases after the start of brain radiation: early (within minutes); early-delayed (within one-to-four months); and late, delayed (beyond four months). For example, some patients may experience headache or confusion, even within minutes of the completion of radiation treatment. This type of reaction is quite rare and these acute side effects of irradiation usually resolve completely without treatment.
Examples of early-delayed side effects which may occur at between one-to-four months after radiation therapy may include the worsening of limb weakness, problems with gait, increasing somnolence, problems with smell or taste, and abnormal sensation or tingling.
Very often, these early-delayed side effects will go away as the tumor continues to shrink. These side effects might improve with the use of powerful steroids such as dexamethasone. In addition, some patients who receive radiation therapy to the neck may experience electric shock-like sensations which radiate from the neck downwards to the arms and/or legs or trunk. These sensations usually only last for a short duration; usually less than a second. This sensation is known as Lhermitte's sign and is usually triggered by flexing the neck forward. When the head moves in this way, the electric shock-like sensations are triggered.
Late radiation toxicities which may occur starting four months after irradiation and beyond include permanent brain injury. Over time, some patients who have had brain irradiation may experience problems with thinking and with memory and require assistance with activities of daily living.
Rarely, the long-term toxicity of brain radiotherapy can cause serious damage known as necrosis - the destruction of both tumor cells as well as small areas of the surrounding brain. This type of toxicity occurs in less than 10% of patients and can be relieved by surgery or by the use of steroids such as dexamethasone.
A new technology for the delivery of brain radiation to treat brain metastatic disease has recently been developed and is called radiosurgery. This is an alternative to whole brain radiation treatment and is especially appropriate for smaller lesions, less than 3-4 cm in diameter. Radiosurgery can be administered by two types of machines, known as either the gamma knife® or the cyberknife.® The gamma knife is a highly sophisticated technique that delivers a high dose of radiation in a finely focused beam to small, intracranial tumor targets. The gamma knife is considered to be minimally-invasive; it is associated with very little discomfort and few immediate side effects. In contrast, the cyberknife is considered to be non-invasive as there is no frame used to immobilize the head of the patient. Instead, cyberknife combines robotics with computer-assisted image guidance to continuously aim the radiation beam at the target. Treatment with the gamma knife is administered in one session; treatment with the cyberknife is delivered over between one-to-five days. Each of these approaches is designed to focus the radiation only on the area of the brain known to harbor the tumor cells, sparing the normal brain as much as possible. Nevertheless, some of the side effects, both short and long-term, sometimes seen after brain irradiation, also occur after stereotactic brain irradiation: Five-to-ten percent of patients treated with radiosurgery may eventually develop necrosis of the irradiated area and possibly require surgery to remove the necrosis. Nevertheless, radiotherapy provides excellent control of a tumor and in some patients is an adequate substitute for surgical removal of the metastatic tumor.
Day of Radiosurgery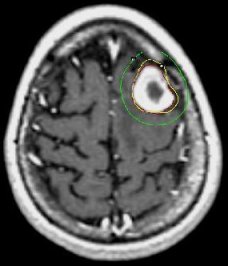
|
5 Months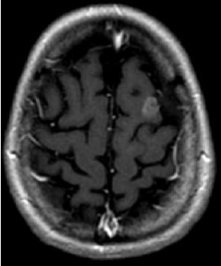
|
3 Years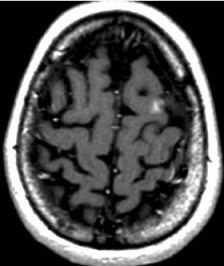
|
| MRI scans of a brain metastasis from breast cancer shown on the day of radiosurgery, 5 months later, and 3 years later | ||
Reference: Roy, S., Josephson, S.A., Fridlyand, J., Karch, J., Kadoch, C., Karrim, J., Damon, L., Treseler, P., Kunwar, S., Shuman, M.A., Jones, T., Becker, C.H., Schulman, H., and Rubenstein, J. L. "Protein Biomarker Identification in the Cerebrospinal Fluid in Patients with Central Nervous System Lymphoma." 2007. In Press, Journal of Clinical Oncology .
|
You are welcome to share this © article with friends, but do not forget to include the author name and web address. Permission needed to use articles on commercial and non commercial websites. Thank you. |